Stem Cell Therapy for Type 1 Diabetes: A Comprehensive Overview
Introduction
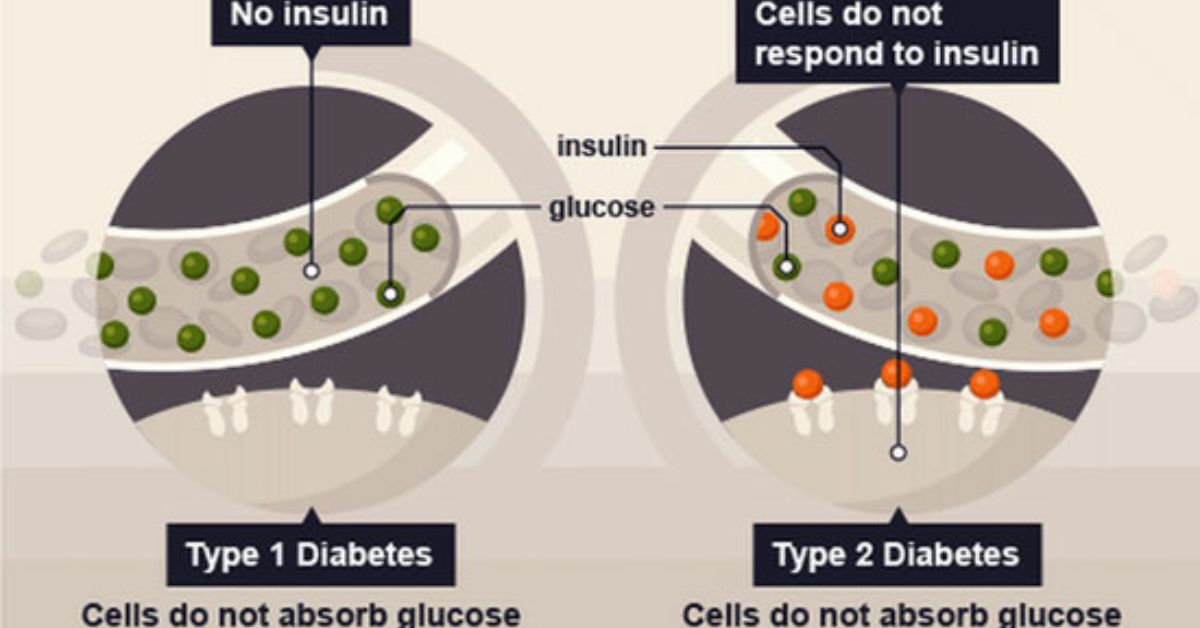
Type 1 Diabetes (T1D) is an autoimmune condition where the body’s immune system mistakenly attacks insulin-producing beta cells in the pancreas. This leads to elevated blood sugar levels and requires lifelong insulin therapy. However, advancements in regenerative medicine, particularly stem cell therapy, offer new hope for those affected by this chronic condition.
What is Stem Cell Therapy?
Stem cell therapy involves using stem cells to repair or replace damaged tissues. Stem cells are unique due to their ability to differentiate into various cell types and self-renew, which makes them a promising tool for regenerative medicine. For Type 1 Diabetes, the goal is to restore the function of insulin-producing cells in the pancreas.
How Stem Cell Therapy Works for Type 1 Diabetes
- Cell Sourcing: Stem cells can be sourced from various places, including the patient’s bone marrow or umbilical cord blood. For T1D, the focus is on differentiating these stem cells into pancreatic beta cells.
- Cell Differentiation: Once harvested, stem cells are cultured in a controlled environment to develop into beta cells. This process involves exposing the stem cells to specific growth factors and conditions that promote their transformation into functional insulin-producing cells.
- Transplantation: The differentiated cells are then transplanted into the patient’s body, typically into the pancreas or nearby tissue. The objective is for these new cells to integrate and begin producing insulin naturally.
- Immune Modulation: Since T1D is an autoimmune condition, patients may also receive treatments to modulate the immune system and prevent it from attacking the newly introduced beta cells.
Benefits of Stem Cell Therapy for Type 1 Diabetes
- Potential for Insulin Independence: Successful therapy may reduce or eliminate the need for external insulin administration.
- Improved Glycemic Control: Enhanced beta cell function can lead to better management of blood sugar levels.
- Reduced Risk of Complications: By achieving better glucose control, patients may lower their risk of diabetes-related complications such as neuropathy, nephropathy, and retinopathy.
Challenges and Considerations
- Success Rates: While promising, the success rate of stem cell therapy for T1D varies. Reports suggest a 50-60% success rate, which depends on factors like disease duration and patient health [1].
- Safety: The therapy involves complex procedures, including cell sourcing and immune system modulation, which carry potential risks and side effects.
- Cost: The cost of stem cell therapy can be significant, and it is often not covered by insurance. Patients should consult with medical professionals to understand the financial implications [1].
Current Status and Future Directions
Stem cell therapy for Type 1 Diabetes is still under research and development. Clinical trials are ongoing to refine techniques, improve success rates, and ensure long-term safety. Advances in technology and a better understanding of immune responses are expected to enhance the effectiveness of this therapy.
Conclusion
Stem cell therapy represents a promising frontier in the treatment of Type 1 Diabetes, offering the potential to restore pancreatic function and improve quality of life. As research progresses, it is hoped that this innovative approach will become a viable treatment option for a larger number of patients.
For those interested in exploring stem cell therapy for Type 1 Diabetes, consulting with specialized medical centers and participating in clinical trials may provide opportunities for early access to this emerging treatment.